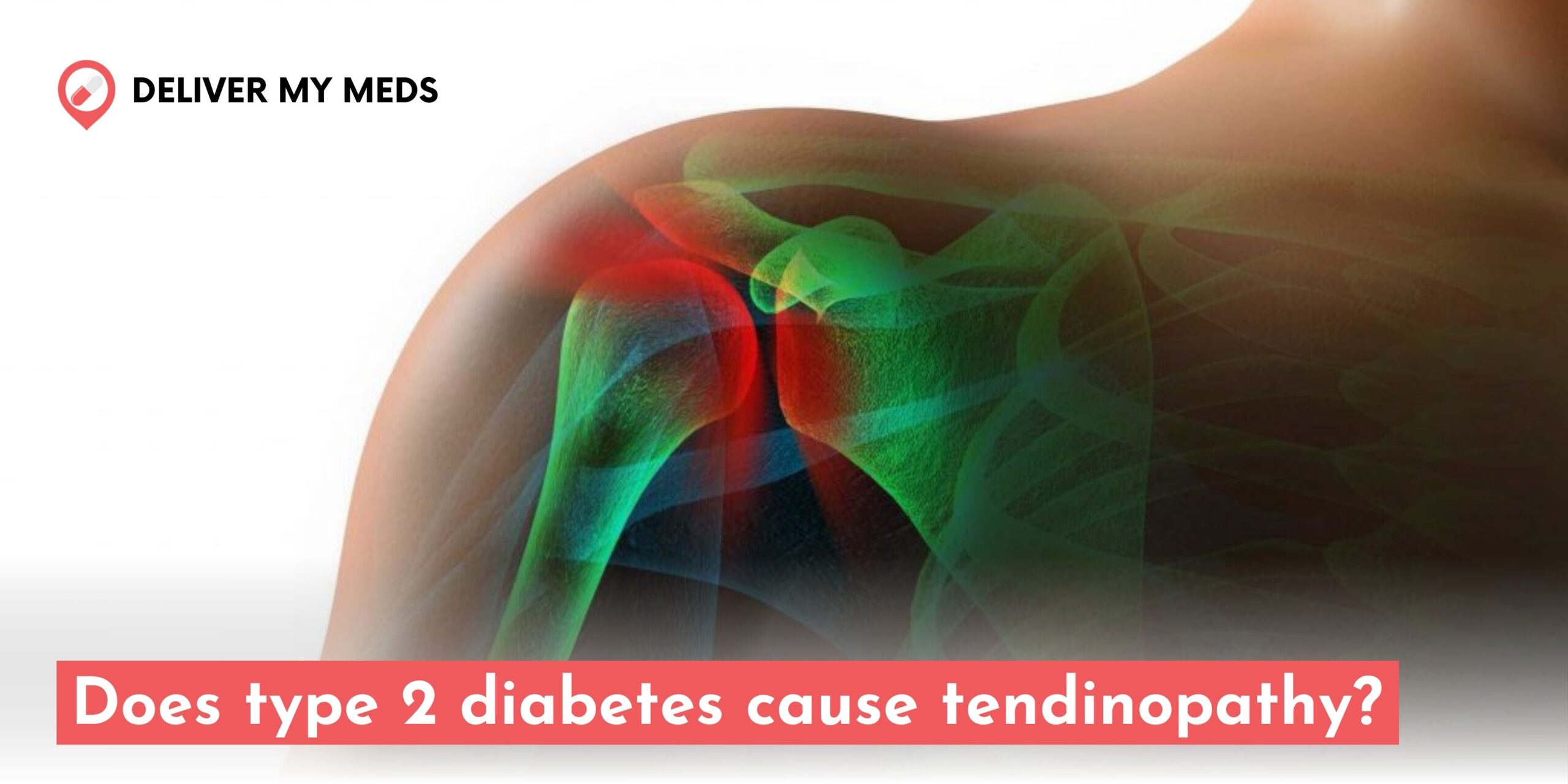
Type 2 diabetes is when the body becomes resistant to insulin or does not produce enough. It can lead to a wide range of complications. While other risks of diabetes, including cardiovascular problems, kidney disorders, and diseases of the eye, are a little older than this study’s focus, recent research has also indicated a concerning link between diabetes and tendinopathy. Tendinopathy refers to the damage of tendons, those fibrous tissues attaching muscles to bones, that leads to pain, swelling, and dysfunction. Let us investigate in detail, “Does type 2 diabetes cause tendinopathy”, exploring some mechanisms responsible and options on how one could prevent this disease or modify it.
What Is Tendinopathy?
Tendinopathy is an over-arching term that describes an injury to a tendon, thus including tendonitis, which means inflammation of the tendon, and tendinosis, which relates to tendon degeneration. Tendons are commonly subjected to repetitive stress or strain, resulting in pain when inflamed or unable to move smoothly. Tendinopathy frequently affects the tendon area in the shoulders, elbows, knees, or Achilles, often making it cumbersome to perform very simple daily activities.
The Link Between Type 2 Diabetes and Tendinopathy
Over the past few decades, medical science has increasingly been pointing to a relationship between Type 2 diabetes and an increased risk of tendinopathy. This connection is thought to be due to several factors inherent to diabetes, such as poor blood circulation, high blood sugar levels, and increased stiffness in the connective tissues.
Here’s how Type 2 diabetes contributes to tendinopathy:
1. Collagen and Tendon Degeneration
Tendons mainly comprise collagen, a structural protein that gives strength and flexibility. The common issue in the tendons of patients with Type 2 diabetes is collagen cross-linking- that is, how collagen fibers link up to create strength. An excess amount of blood glucose causes overproduction of advanced glycation end-products (AGEs) and has been shown to cause damage to the collagen fibers. With decreased function because of a damaged collagen structure, the tendons become more vulnerable to wear and tear, resulting in tendinopathy.
2. Poor Blood Circulation
People with Type 2 diabetes have an increased risk of vascular problems due to years of damage from high blood sugar. Typically, impaired circulation affects the tendons since they rely on good circulation to heal normally. Tendons might fail to repair from minor injuries due to insufficient blood supply. Consequently, it leads to chronic inflammation and degeneration, which is typical of the condition known as tendinopathy.
3. Increased Inflammation
Chronic inflammation is characteristic of Type 2 diabetes and can contribute heavily to the issues of the tendons. Hyperglycemia leads to systemic inflammation that, while damaging to tissues in other parts of the body, often impacts the tendons. Pain, swelling, and stiffness result from inflammation of the tendon, all contributing to the formation of tendinopathy.
4. Loss of Tendon Elasticity
Another problem is tendon stiffness in Type 2 diabetes patients. Over time, high glucose levels make tendons and other connective tissues less flexible by interacting with the proteins in the body and forming abnormal cross-links. The likelihood of tendon strain and injury with tendinopathy increases due to this reduced flexibility.
Common Sites of Tendinopathy in Type 2 Diabetes Patients
Diabetes-associated tendinopathy can affect the tendons of any part of the body. These include, amongst others:
- Achilles tendon: The back of the ankle is particularly associated with tendinopathy in diabetic patients. This is the tendon from the calf to the heel bone.
- Shoulder tendons: The latter tend to suffer from tendinopathy in persons with a prolonged elevation of blood sugar and subsequently cause shoulder pain and limited movement.
- Hand flexor tendons: Tendon problems may be affected across the hands, especially in poorly managed diabetes.
- Patellar tendon: A structure of the knee, this tendon may also increase vulnerability to tendinopathy, especially when a person who suffers from diabetic vascular complications experiences it.
Risk Factors for Tendinopathy in Type 2 Diabetes
Some risk factors can increase the likelihood of developing tendinopathy in patients with Type 2 diabetes:
- Poorly controlled blood sugar: High glucose levels can worsen tendon damage over time.
- Obesity: Type 2 diabetic patients are prone to overweightness or obesity, causing excess weight strain on tendons.
- Age: Tendons deteriorate at an age even without any ailment; moreover, complications through diabetes would surely exacerbate their deterioration.
- Lack of physical movement: Limpness of bones and muscles leads to weaker and more susceptible injury-prone areas.
- Duration: The longer they lived with Type 2 diabetes, the greater the amount of exposure over time to uncontrolled levels of blood sugar.
Symptoms Tendinopathy
Depending on location and the severity, tendinopathy can come with several symptoms, such as:
- Pain in the involved tendon is worse when moving or using the joint.
- Swelling around the tendon
- Stiffness that presents difficulty in the movement of the joint.
- Weakness associated with the affected limb or joint.
- Tenderness when applying force to the tendon.
Preventing and Managing Tendinopathy in Type 2 Diabetes
There are measures taken by people who have Type 2 diabetes that will help decrease the chances of acquiring tendinopathy and will assist in the management of tendinopathy when it occurs. They include the following:
1. Control of Blood Sugar
Control of blood sugar levels is the most potent measure to avoid complications, which may include tendinopathy. A healthcare provider can control it through diet, exercise, and medication.
2. Continuously monitor your Glucose
In managing diabetes, a valuable tool would be the ability to track one’s glucose continuously in real-time, both during the day and at night, using CGM. The latter does not like the traditional fingerstick test. It will give a continuum and more accurate information about patterns and trends. Continuous monitoring thus helps improve diabetes management overall. Blood glucose can be better managed, and the risks of developing complications could be reduced. Other widely used CGM devices are Abbott’s Freestyle Libre, Dexcom G6 from Dexcom, and Guardian Connect from Medtronic. These are mainly those stuck on the skin, and the data would be sent to a phone or the receiver, where the users will make far better decisions regarding diet, activity, and insulin use.
3. Exercise regularly
Tendon strength and flexibility can be enhanced through regular physical activity. Therefore, one would be on a good preventive measure against injury through low-impact exercises, which include walking, swimming, and cycling, which do not strain the tendons too much. Stretching exercises that improve flexibility are also significant for tendon health.
4. Weight Management
Maintaining a healthy weight reduces the load on tendons, especially in the lower body, and will thus tend to reduce the likelihood of tendinopathy. If you have excess weight, losing weight slowly through diet and exercise will be useful.
5. Early intervention
If you develop symptoms such as pain or swelling of a tendon, seek early medical advice. Early diagnosis and treatment can prevent further damage to the tendon and help prevent long-term complications.
6. Physical Therapy
A physical therapist can help guide you through exercises that strengthen the tendons, help you achieve flexibility, and minimize the risk of injury. In addition, they can offer recommendations for special exercises to treat existing tendinopathy.
7. Anti-inflammatory Drugs
The patient who is suffering from the pain and swelling caused by tendinopathy will be relieved of the condition if treated with the help of a doctor using NSAIDs.
8. Surgery (in rare cases)
When conservative treatments have failed, there is a slight chance that one may require surgical intervention to treat the tendon. However, such a scenario should be considered the last option unless tendinopathy has resulted in significant disability.
Conclusion
Poor blood circulation, damage to collagen, increased inflammation, and tendon stiffness increase the risk of developing tendinopathy with Type 2 diabetes. However, this relationship presents a challenge; controlling blood sugar levels, staying active, and taking steps to reduce strain on tendons can help prevent or minimize the impact of tendinopathy. Early diagnosis and treatment can effectively manage the condition, thereby ensuring a better quality of life between diabetes and tendon injuries. So, if you have Type 2 diabetes, then talk to your doctor immediately if you find symptoms of tendinopathy to prevent further complications from building up.